Utilising musculoskeletal ultrasound allows us to effectively visualise and diagnose various musculoskeletal conditions and efficiently treat one joint or multiple joints with cellular prolotherapy immediately or thereafter in cases that warrant this type of treatment protocol.
Diagnosing and treating injured and degenerative joints is an added bonus in particular aspects of patient care. The use of ultrasound will not replace palpation or clinical examination of the painful joint, but may be used as a tool to compliment the expertise at hand. Ultrasound guidance can be used before treatment to assess and diagnose, or during treatment to inject directly into the injured joint structures, and after treatments, once tissue/joint remodelling has occurred, to document the successful healing outcomes.
What Is Ultrasound?
Ultrasonography is an imaging modality that uses high frequency sound waves, which normally cannot be heard by human beings, to visualize internal structures of the body. “Ultrasound travels as sound waves, and images are generated when pulses of ultrasound from the transducer produce echoes at tissue or organ boundaries. Between pulse transmissions, the transducer serves as a detector of echoes, which are processed to form an anatomic image.”2 The waves are recorded and made into images, allowing us to visualize structures such as tendons, muscles, ligaments, and more. “Interpretation of the ultrasound images depends on the echogenicity: the brightness of the image, depending on the degree of reflection in the ultrasound waves.”2
At this office we are using the GE Logiq e, portable point-of-care ultrasound machine.

GE Logiq e Ultrasound
The Benefits of Using Ultrasound in Treating Chronic Pain
Ultrasound is attractive to patients because of its safety! It is non-invasive, painless, convenient, and free of radiation! Other benefits include: Potential to show and document improvement in soft tissue injuries and track patient objective outcomes from Prolotherapy treatments utilising before and after images. Is able document musculoskeletal pathology, as studies suggest that ultrasound is the primary imaging technique for soft tissue injuries.2
The ability to achieve greater sensitivity in diagnosing rotator cuff injuries - “Rotator cuff issues are very common and is one of the most common reasons for using ultrasound. Many studies report excellent sensitivity and specificity of ultrasound in diagnosing rotator cuff tears.”2
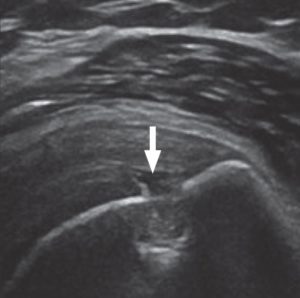
Ultrasound scan of shoulder showing supraspinatus tear (arrow).
Ultrasound Diagnosis and Treatment aid in Tendon Degeneration and Tears.
Tendon degeneration on ultrasound is seen as irregularities of fibrillar appearance, such as thickening and fragmentation, with focal hypo echoic areas, and calcifications.
“Dynamic imaging deserves special emphasis because it is useful in differentiating full-thickness from partial-thickness tendon tears, muscle tears, and tendon subluxations or dislocations.”3
It is possible to accurately visualise and diagnose tendon tears of the upper and lower extremities. As for example, studies reported an accuracy of 94% when ultrasound was used to diagnose tendon tears of the ankle.3
The ability reveal altered anatomy after surgery becomes more apparent. In many post-surgical cases, a patient’s anatomy may be altered slightly. Ultrasound is effective for evaluation of soft tissue near metal hardware, which may include metal screws, plates, etc.

Ultrasound of lateral ankle showing anterior talofibular ligament tear (arrow).
In certain instances, anatomy may be relocated, such as in the case of the ulnar nerve in the elbow, which may be relocated as part of a surgical procedure. Ultrasound is able to help visualise the altered anatomy. “Ultrasound applications are not limited to, but include evaluation of peripheral nerves, evaluation for soft-tissue foreign bodies and the evaluation of soft-tissue abnormalities adjacent to hardware.”3
- The ability to monitor needle positioning during the injection procedures paramount. For example, injections into joints such as the hip, as well as soft tissue injections into the tendons, ligaments and other joint structures.
- Ultrasound can also be performed during motion. Unlike an MRI, ultrasound can be performed on a patient while joints are in motion. In cases of shoulder impingement, for example, a patient may only have pain with certain motions and none at rest. Ultrasound can help visualize what happens with the tissue during motion. “The main advantages are its ability to perform dynamic examinations and to conduct side-to-side comparisons on the spot, allowing clinicians to correlate their patients’ symptoms directly with anatomic visualization.”3“Studies have shown ultrasound to be accurate in the diagnosis of conditions that require joint movement or positioning to display the abnormality, such as peroneal tendon subluxation in the ankle (100% positive predictive value). Such diagnoses are not possible or are difficult with routine MRI.”3
- Are there any disadvantages to using Ultrasound? The main disadvantage is operator dependence. The same holds true for MRI, X-ray and any other diagnostic tool. Ultrasound must be used as an adjunct to treatment. Palpation, physical exam, patient history and practitioner expertise are paramount.
Ultrasound Guided Joint Injections
Ultrasound allows us to visualize musculoskeletal tissue. We can visualize the injured tissue right in the office without having to wait for an MRI. During treatment, we can inject the injured structures and maintain continued needle visualization of the targeted areas.
Ultrasound guided treatment is not used on every patient. Ashmore Osteopathic Group (AOG) has been a practicing Prolotherapy clinic for many years without the use of image guidance for injections using the palpation guided technique.
The Prolotherapists at AOG along with many other practitioners have been using this same treatment method. During this time, thousands and thousands of patients have had their pain levels improve dramatically without the addition of ultrasound.
The many benefits of ultrasound are noted above; however, we try to keep our Prolotherapy related costs as low as possible. Any added cost can be a financial burden to patients, especially those who require many treatments or those who have multiple joints treated.

The decision to use ultrasound guidance is based on the needs of the individual patient and is not a rule for all.
As a prominent Prolotherapy clinic on the Gold Coast, we see a lot of the more complicated cases. People generally come to us in pain! They have frequently seen numerous practitioners, received numerous procedures, tried multiple medications and have been subjected to one or multiple surgeries. If their anatomy has been changed due to surgery, with ultrasound we can safely localize the altered anatomy, implants, screws and rods, and then treat the injured or degenerated joint(s).
As ultrasound allows visualisation of pathology during motion, this means that we can watch the ligaments and tendons around the joint through ultrasound as you move. With ultrasound, the patient can perform the motion that elicits the pain, while we visualize the joint and joint structures. This allows us to see directly and immediately, any changes that occur in the anatomy during the motion that exhibits pain. We can then treat the visualized musculoskeletal condition with Prolotherapy.
As you know, the Prolotherapists at AOG do not rely on MRIs or other imaging. However, in certain cases imaging may be deemed necessary, but some patients may not be able to get an MRI due to metal implants in their body. If someone has a metal implant from a previous surgery, we can still perform ultrasound to help visualize the pathology. Also, in complicated cases, imaging may be advantageous, so having the availability of ultrasound is a valuable option.
How Does Ultrasound Compare to MRI
Ultrasound has significant advantages over MRI, specifically in regards to dynamic imaging, or imaging while the joint is in motion. For example, we can evaluate external rotation of the shoulder to diagnose a tendon dislocation or arm elevation to diagnose an impingement or adhesive capsulitis. The elbow can be flexed to diagnose snapping triceps syndrome. Visualization of movement in the hip can diagnose snapping hip syndrome. Ultrasound imaging of the ankle can aid in diagnosing a tendon subluxation or tear.
- Various studies have found comparable accuracy of diagnostic ultrasound and magnetic resonance imaging for diagnosis and measurement of rotator cuff tears.2,3
- “One limitation of ultrasound is the inability of the ultrasound beam to penetrate beyond bone cortex. Although ultrasound can evaluate some aspects of joint cartilage, MRI offers a more comprehensive evaluation of those structures. Nonetheless, much of the musculoskeletal system can be evaluated with ultrasound.”3
- As in any field, there are variables with equipment, training and experience. High accuracy can be obtained with proper training and use of appropriate equipment. The ultrasound professional must understand anatomy. Prolotherapists, who have been palpating painful joint for years, understand anatomy as well as referral patterns. The Prolotherapist trained in ultrasound technology can also adequately evaluate structures in a standardized imaging plane, recognize artifacts and correct for them, recognize abnormalities in the image, and finally interpret the imaging findings. When comparing to MRI, the MRI technologist must be properly trained as well. A possible benefit of MRI over ultrasound is the use of intra-articular contrast material to boost reporting accuracy for tears while using MR
arthrography.3“Ultrasound is an ideal and inexpensive alternative for imaging structures, such as tendons, ligaments, and peripheral nerves of the distal extremities as well as for evaluation for soft-tissue foreign bodies. Compared with ultrasound, MRI offers a more comprehensive evaluation that includes intra-articular structures, bone marrow, and deep soft tissues.”3In summary, ultrasound is a simple and safe, radiation-free modality that offers convenience of musculoskeletal assessment right in the practitioners office. The physician can palpate the injured area, utilise ultrasound to link the imaged area with the patient’s subjective symptoms and pathology, and then treat the visually confirmed musculoskeletal condition with Dextrose Prolotherapy, PRP Prolotherapy, or Stem Cell Prolotherapy. As treatment progresses, ultrasound offers the ability to document the clinical changes, repair and healing of the treated structures.
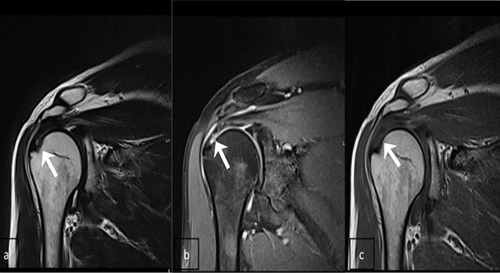
MRI Shoulder
References:
1.Kane D, Balint PV, Sturrock R, Grassi W. Musculoskeletal ultrasound—a state of the art review in rheumatology. Part 1: Current controversies and issues in the development of musculoskeletal ultrasound in rheumatology. Rheumatology. 2004; 43 (7): 823-828.
2.Lew HL, Chen CPC, Wang T-G, Chew KTL. Introduction to musculoskeletal diagnostic ultrasound: examination of the upper limb. Am J Phys Med Rehabil. 2007;86:310–321.
3.Jacobson JA. Musculoskeletal Ultrasound:Focused Impact on MRI.AJR 2009; 193:619–627.